Page 74 - DR.BROCHURE 2019_
P. 74
Red M. Alinsod, M.D., FACOG, FACS, ACGE 74
In the News
Radiofrequency resurfacing:--- 22/01/14 15:25 Pagina 106
Radiofrequency resurfacing:--- 22/01/14 15:25 Pagina 107
Aesthetic gynecologic surgery Radiofrequency resurfacing and revision of deepithelialized labia minora labiaplasty: review of literature and case study
Radiofrequency resurfacing and revision of deepithelialized
labia minora labiaplasty: review of literature and case study
RED ALINSOD
Urogynecology Director, The Women’s Center and The Laguna Laser Center, South Coast, CA
Abstract: The growing demand for Aesthetic Vulvo-vaginal Surgery (AVS), particularly elective and therapeutic labia minora plasty (labia mi-
nora reduction) procedures, has increased the risk of failed labiaplasties when performed by inexperienced or poorly trained surgeons.
Inadequate labia minora reduction surgery may result in medical and functional complications as well as aesthetically unattractive results.
Complications of a botched labiaplasty include bleeding, infection, delayed wound healing, iatrogenic asymmetry, and under or overcorrec-
tion. This case report illustrates the use of an innovative radiosurgical technique to repair poor anatomical outcomes of an unsuccessful de-
epithilialized labia minora plasty. Revision surgery was achieved using a radiofrequency device that allows incision, micro-smooth cutting,
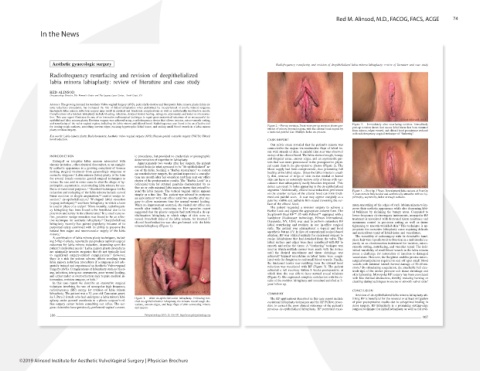
and resurfacing of the vulva-vaginal region, including the labia minora and clitoral hood. Radiofrequency was found to be an effective tool Figure 3. – Immediately after resurfacing revision. Immediately
for ironing rough surfaces, smoothing uneven edges, excising hypertrophic labial tissue, and sealing small blood vessels in a labia minora Figure 2. – Pre-op revision. Front view pre-op revision shows pro- post-op revision shows that excess labial tissue has been trimmed
plasty revision surgery. trusion of minora beyond majora, with the clitoral hood topped by from minora, edges evened, and clitoral hood prominence reduced
a hardened painful scar. Multiple holes are present. with radiofrequency surgical technique of “flathering”.
Key words: Labia minora plasty; Radiofrequency; Aesthetic vulvo-vaginal surgery (AVS); Female genital cosmetic surgery (FGCS); Clitoral
hood reduction. CASE REPORT
Our pelvic exam revealed that the patient’s minora was
connected to the majora via unattractive flaps of labial tis-
sue with strands of skin. A painful firm scar was observed
INTRODUCTION ic procedures, but provided no credentials or photographic on top of the clitoral hood. The labia showed rough, bumpy
and irregular areas, uneven edges, and an asymmetric pat-
Enlarged or irregular labia minora associated with documentation of expertise in labiaplasty. tern that was more pronounced in the postoperative physi-
chronic irritation, other physical discomfort, or an unsight- Approximately two weeks after her surgery, the patient cal exam than in the pre-operative photos (Figure 2). The
ly aesthetic appearance is a growing complaint of women noticed holes in what appeared to be “de-epithelialized” ar- blood supply had been compromised, thus preventing full
eas of the labia. Seeking a “Barbie Appearance” to correct
seeking surgical treatment from gynecologic surgeons or healing at the labial edges. Since the labia minora is usual-
cosmetic surgeons. 1 Labia minora (labia) plasty is the term an unsatisfactory surgery, the patient requested a consulta- ly thin, removal of strips of skin on the medial or lateral
for several female cosmetic genital surgical techniques to tion one month after her operation and then sent our office side can leave an extremely narrow strip of tissue with vas-
reduce the size and in some cases to alter the shape of hy- photos of the postoperative results. The “Barbie Look” is a culature that subsequently easily becomes impaired. This
colloquial term for external genitalia characterized by ei-
pertrophic, asymmetric, or protruding labia minora for aes- defect can result in holes appearing in the de-epithelialized
thetic or functional purposes. 1-2 Standard techniques for the ther no or only minimal labia minora tissue that extend be- segments. 9 Additionally, clitoral hood reductions performed
reduction and reshaping of the labia minora include curved yond the labia majora. The vertical vaginal orifice appears on the anterior surface of the clitoral hood can form thick- Figure 4. – Post Op 3 Years. Resculptured labia minora at Post Op
3 years remain fully healed and aesthetically attractive with no hy-
linear excision or simple amputation, 3-4 central wedge re- simply as a fine line. The patient was advised to postpone ened and painful scars. A scar may appear unsightly as a pertrophy, asymmetry, holes or rough surfaces.
an appointment with our office until two months after sur-
section, 5 de-epithelialization, 6 W-shaped labial resection pale but visible and palbable firm strand traversing the sur-
(zigzag technique), 7-8 and laser labiaplasty in which a laser gery to allow maximum time for normal wound healing. face of the clitoral hood.
is used in place of a scalpel. 1 More recently, radiofrequen- When no improvement occurred, she visited our office one The patient requested a revision surgery to achieve a mum smoothing of the edges of each labium minora to im-
prove their aesthetic appearance while also decreasing labi-
cy labiaplasty has been found to be beneficial due to its month after initially contacting us. Her operative report Barbie Look and signed the appropriate consent form. The al bulkiness by shrinking the bumpy areas. Compared to
suggested that the plastic surgeon had performed a de-ep-
precision and safety in the clitoral area. 9 In a small case se- Surgitron® Dual RF™ S5 with Pellevé™ equipped with a
ries, posterior wedge resection was found to be an effec- itheliazation labiaplasty in which strips of skin were re- handpiece (Radiowave technology, Ellman International, lower frequency electrosurgery instruments, monopolar RF
tive technique for aesthetic labiaplasty. 10 Deepithelialized moved from both sides of the labia minora. An inverted U Oceanside, NY, USA) was used to perform sutureless RF treatment is associated with decreased tissue resistance and
maximum control in precision cutting as well as tissue
labiaplasty recently has gained popularity because of its clitoral hood reduction was also performed with the labia labial resurfacing and revision in our in-office surgical tightening to smooth wrinkled skin. 9 This technique is ap-
minora labiaplasty (Figure 1).
purported safety combined with its ability to preserve the suite. The patient was administered a topical and local
natural free edges and neurovascular supply of the labia anesthetic but no I.V. In lieu of conventional scalpel-based propriate for corrective labiaplasty cases requiring delicate
minora. 1 ablation, RF was utilized initially for excisional surgery to and meticulous repair of labial tissue and vasculature.
The versatility of radiosurgery with its detachable hand-
A combination of labia minora plasty techniques, includ- excise labial tissue that had detached from the vulva. The
ing 5-flap Z-plasty, reportedly can produce optimal surgical labial surface and edges were then resurfaced with RF to piece hair wire tips allows it to function in a multimodal ca-
outcomes for labia minora reduction, depending upon the smooth and refine the tissue. A “feathering” techique was pacity as an electrosection instrument for incision, micro-
patient’s individual needs. 1 Labia minora plasty procedures used in which multiple passes were made with the device smooth cutting, resurfacing, and vascular repair. The indi-
vidual variability of small blood vessels in the labia minora
are minimally invasive surgeries that do not typically lead until the desired smoothness and tissue shrinkage was poses a challenge for restoration of function to damaged
to significant surgery-related complications. 3 However, achieved. 9 Injured vasculature in labial tissue were coagu-
there is a risk for serious adverse effects resulting from lated with the Surgitron to seal small blood vessels. Finally, vasculature. However, the Surgitron enables precise micro-
labia minora reduction procedures if a surgeon is not ade- the thickened tender scar resulting from the clitoral hood surgical manipulation required to seal off open small blood
vessels with minimal lateral thermal damage of 20-40 mi-
quately trained and experienced in Aesthetic Vulvo-vaginal reduction was resurfaced with RF (Figure 3). The patient crons. 9 By stimulating coagulation, the attachable ball elec-
Surgery (AVS). Complications of labiaplasty such as bleed- achieved a full recovery within 8 weeks postoperative at
ing, infection, iatrogenic asymmetry, poor wound healing, which time she was able to have normal sexual relations trode tips of the device promote soft tissue shrinkage and
and either under or overcorrection may require medical in- (Figure 4). She expressed complete satisfaction with the re- skin tightening. Monopolar RF surgery has been associated
with less thermal destruction, thereby reducing burning or
tervention, revision surgery, or both. 1 sults of the revision labiaplasty and remained satisfied at 3- charring during techniques to excise or smooth vulvar skin. 9
In this case report we describe an innovative surgical year follow up.
technique involving the use of monopolar high frequency
radiofrequency (RF) energy for revision of labia minora CONCLUSION
labiaplasty. The patient was a 32 year-old Caucasian gravi- COMMENT Revision of de-epithelialized labia minora labiaplasty uti-
da 3, Para 2 female who had undergone a labia minora labi- Figure 1. – After de-epithelialization labiaplasty. Following bot- The RF applications described in this case report include lizing RF is beneficial for the reversal or at least mitigation
aplasty under general anesthesia in a plastic surgeon’s of- ched de-epithelialization labiaplasty the minora reveal rough ele- excisional labiaplasty techniques and the RF Pelleve proce- of poor postoperative results due to suboptimal healing in
fice surgery center before consulting our office. The sur- vations, uneven edges, and large flaps of skin connecting minora dure to correct the poor clinical outcomes of the patient’s prior surgery. RF labiaplasty is a promising cutting-edge
geon claimed to have previously performed vaginal cosmet- and majora.
previous de-epithelialized labiaplasty. RF permitted maxi- surgical technique for initial labiaplasty as well as for revi-
106 Pelviperineology 2013; 32: 106-109 http://www.pelviperineology.org
107
©2019 Alinsod Institute for Aesthetic VulvoVaginal Surgery | Physician Brochure